"As “Collaborating Physician Agreements: Legal Mistakes to Avoid” takes center stage, this opening passage beckons readers with casual formal language style into a world crafted with good knowledge, ensuring a reading experience that is both absorbing and distinctly original."
"The content of the second paragraph that provides descriptive and clear information about the topic"
Overview of Collaborating Physician Agreements
Collaborating Physician Agreements are crucial legal documents that Artikel the relationship between a primary physician and a collaborating physician. These agreements are essential in healthcare settings where multiple providers may be involved in a patient's care to ensure clarity, accountability, and compliance with legal regulations.
Purpose of Collaborating Physician Agreements
Collaborating Physician Agreements serve to establish the roles and responsibilities of each physician involved in the care of a patient. They help define the scope of practice, communication protocols, and decision-making processes to ensure seamless coordination of care.
- Clearly Artikel the duties and obligations of each physician
- Specify the scope of practice and limitations for the collaborating physician
- Establish communication protocols for sharing patient information and coordinating care
- Ensure compliance with legal and regulatory requirements
Key Components of Collaborating Physician Agreements
Collaborating Physician Agreements typically include the following key components:
- Identification of the primary physician and collaborating physician
- Scope of practice for the collaborating physician
- Duration of the agreement and termination terms
- Communication protocols and information sharing guidelines
- Provisions for compliance with state laws and regulations
Importance of Collaborating Physician Agreements
Having Collaborating Physician Agreements in place is essential for several reasons:
"These agreements help clarify the roles and responsibilities of each physician, promote effective communication, ensure compliance with legal requirements, and ultimately enhance the quality of patient care."
By outlining expectations and guidelines for collaboration, these agreements mitigate potential conflicts, reduce legal risks, and improve the overall coordination of care for patients.
Common Legal Mistakes in Collaborating Physician Agreements
When drafting collaborating physician agreements, healthcare providers often make common legal mistakes that can have serious consequences for all parties involved. These errors can range from vague language to overlooking important details, leading to potential disputes and legal issues down the line.
Ambiguity in Roles and Responsibilities
One of the most common mistakes in collaborating physician agreements is ambiguity regarding the roles and responsibilities of each party. When the terms of the agreement are unclear, it can lead to misunderstandings, conflict, and ultimately, legal disputes.
- Example: Instead of clearly outlining the specific duties of the collaborating physician, using vague language such as "assist as needed" can create confusion about expectations.
- Consequence: Ambiguity in roles and responsibilities can result in disagreements over workload distribution, patient care decisions, and financial obligations, potentially leading to breach of contract claims or professional liability issues.
Lack of Termination Clause
Another common mistake is the omission of a termination clause in the agreement. Failing to address how the agreement can be terminated can leave parties in a difficult position if the collaboration needs to end unexpectedly.
- Example: Not including a clause detailing the process for termination, including notice period and reasons for termination, can leave both parties vulnerable in case of disputes.
- Consequence: Without a clear termination clause, parties may find themselves in protracted legal battles or facing financial repercussions if one party decides to end the collaboration abruptly.
Inadequate Confidentiality Measures
Failure to establish robust confidentiality measures is another common legal mistake in collaborating physician agreements. Protecting sensitive patient information and proprietary data is crucial in healthcare settings.
- Example: Using generic language in confidentiality clauses without specifying the types of information to be protected or the measures to safeguard it can leave loopholes for data breaches.
- Consequence: Inadequate confidentiality measures can result in violations of HIPAA regulations, patient privacy breaches, and legal actions for negligence or breach of confidentiality.
Compliance Requirements and Regulations
Collaborating physician agreements in healthcare are subject to a complex regulatory framework that governs the relationships between physicians and other healthcare providers. It is crucial for healthcare organizations to understand and adhere to these compliance requirements to avoid legal pitfalls.
Regulatory Framework for Collaborating Physician Agreements
Healthcare organizations must comply with various laws and regulations when entering into collaborating physician agreements. These may include state-specific regulations, federal anti-kickback statutes, Stark Law, and regulations set forth by accrediting bodies like The Joint Commission.
Ensuring Compliance with Relevant Laws
- Ensure all collaborating physician agreements are in writing and clearly Artikel the roles, responsibilities, and expectations of each party involved.
- Regularly review and update agreements to reflect changes in regulations or healthcare practices.
- Conduct regular audits to ensure compliance with laws and regulations governing collaborating physician agreements.
- Provide ongoing training to staff and physicians on compliance requirements and best practices.
Implications of Non-Compliance
Non-compliance with regulations governing collaborating physician agreements can have serious consequences for healthcare organizations. This may include legal penalties, fines, loss of accreditation, damage to reputation, and even criminal charges in severe cases. It is essential for organizations to prioritize compliance to avoid these negative outcomes.
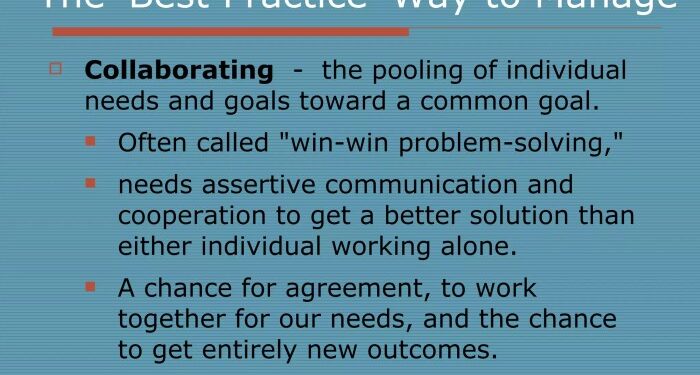
Best Practices for Drafting Effective Agreements
When creating collaborating physician agreements, it is crucial to follow best practices to ensure clarity and enforceability. By incorporating specific language and strategies, you can enhance the effectiveness of these agreements and address potential conflicts proactively.
Use Clear and Specific Language
- Clearly Artikel the roles and responsibilities of each party involved in the agreement.
- Define key terms and expectations to avoid misunderstandings or misinterpretations.
- Include details on patient care protocols, communication methods, and decision-making processes.
Include Enforceable Provisions
- Specify termination clauses, including reasons for termination and notice periods.
- Address confidentiality and data protection measures to protect sensitive information.
- Establish dispute resolution mechanisms to handle conflicts professionally and efficiently.
Implement Regular Review Processes
- Schedule periodic reviews of the agreement to ensure it remains up-to-date and reflective of current practices.
- Allow for amendments or modifications when necessary to adapt to changing circumstances or regulations.
- Encourage open communication between parties to address any concerns or issues promptly.
Final Review
"The content of the concluding paragraph that provides a summary and last thoughts in an engaging manner"
Essential FAQs
"What are some common errors in collaborating physician agreements?"
"Common errors include vague language, lack of specificity, and not addressing potential conflicts upfront."
"How can healthcare organizations ensure compliance with regulations in these agreements?"
"Healthcare organizations can ensure compliance by regularly reviewing agreements, staying updated on relevant laws, and seeking legal advice when needed."
"What are the potential consequences of non-compliance with regulations in collaborating physician agreements?"
"Non-compliance can lead to legal penalties, loss of reputation, and disruption in the provision of healthcare services."